Refuse To Sink
Saturday, November 15, 2025
Refuse To Sink
Nurse Thyself; navigating the aging process as best and as long as we can, while keeping body, mind, and spirit intact.

“Caring is the essence of nursing.” — Jean Watson.
You do not need a nursing degree to become your own best nurse. But you do need something else, something that is a lot more important than any degree available in the scholastic sense. It is called self-compassion.
According to this article, “Self-compassion in practice”, published in American Nurse Journal and written by Erin Lundeen, DNP, RN, CSN, and Connie Perkins, PhD, RN, CNE, they share,
“Self-compassion is a form of self-care that may help increase joy, job satisfaction, and quality of life as well as decrease stress, anxiety, and burnout.”
Resting on the laurels of a three-decade critical care nursing experience, I know this to be true. I am an expert on the nursing self-compassion subject. Along with the thousands of nurses that I worked with throughout the years, we learned the hard way. Nurses and patients alike are better off when we practice self-compassion and self-care. This is evidence based; backed by science.
Self-compassion, self-care, and nurses
Nurses around the world play a significant role in caring for patients, both inside and outside of hospitals. There is no secret that nurses regularly work under extreme stressful conditions; patient overload, long shifts, difficult family members, and staff shortage. A great number suffer from burnout.
The term burnout is not limited to, but includes nurses suffering from work-related depression, feeling overwhelmed, poor physical and mental health, weight gain, moral negativity, difficulty sleeping, and a lack of job satisfaction, according to this peer-reviewed paper published by the National Library of Medicine.
In older adults, burnout is often described as fatigue. Some of the burn out symptoms, experienced by nurses, apply to boomers and our older sisters and brothers as well. Of course, fatigue can be a normal response to physical or emotional stress. It can also be from plain boredom. Or it could be a sign of something more profound.
The National Institute on Aging informs us that fatigue in older adults can be the first sign that something is wrong in the body. Fatigue in older adults is not limited to, but can be the result of chemotherapy and radiation treatment, unmanaged chronic diseases like diabetes, heart disease, arthritic pain, and medication. Depression and loneliness are also common among us in the aging population.
Everyone feels overwhelmed, tired, and out of sync sometimes. But the term burnout is most often connected to caregivers and nurses.
Multiple papers have been written about nursing burnout and how it affects nursing morale and the quality of patient care. Less attention has been given to self-compassion and self-care in nurses and why it matters. Finally, that is changing.
This study used a sampling method to conduct a cross-sectional online survey of 844 clinical nurses from four different hospitals. Participants answered questions that included a Self-compassion scale. The study was aimed at addressing the influence of self-compassion and work engagement, especially from the perspective of moral resilience. My personal take on this is the following;
“Learn to swim by arming ourselves with self-care and stress management techniques to build resilience and mitigate buckling under when feeling overwhelmed, while remaining true to our integrity and moral standards. Get the job done, with help when necessary, and refuse to sink.”
Not surprisingly, the results of the above study showed a significant, positive connection between clinical nurses’ self-compassion and moral resilience. Mediation analysis showed that moral resilience partially mediates the relationship between clinical nurses’ self-compassion and work engagement.
Work engagement is not only the job nurses do to take care of their patients, but it is also the job you and I do to take care of ourselves. Since I am a retired nurse, the latter applies to me as well.
Self-compassion + Self-care = a very good thing.
Now we know that self-care is the essential input needed in order to produce output that is valuable to human well-being. But how do we get to that point? What is the practice of self-compassion and self-care?
The practice of self-compassion and self-care.
Besides bubble baths, breakfast in bed, eating chocolate, and being absorbed reading an intriguing novel, what does the practice of self-care look like?
That answer, my dear reader, is blowing in the wind. Because we are all different, the answers varies from person to person. Chances are, you may already know what self-care looks like for you. If you don’t know, I will help you out with the basics of self-nursing. Remember; I am the expert, having travelled up and down this road as a nurse and as an aging woman.
First, I will tell you what self-compassion looks like for nurses.
In the first-mentioned article about “Self-compassion in practice”, written by two nurses and published in the American Nurse Journal, the authors present a list of suggested self-compassion practices for nurses. Nurses ought to engage in some of these practices when possible.
Here is their helpful list, copied from the article. If some of these suggestions speak to you, take note. This is what Erin Lundeen and Connie Perkins shared in their comprehensive article. Keep in mind; they are both nurses. Their guidance is based on personal experience and research.
Compassion with equanimity
When possible, take time to engage in this self-compassion practice.
- Imagine a person (in your personal or professional life) whom you provide care for.
- The situation is stressful. You’re getting tired, and you may be experiencing some burnout.
- Get in touch with the feelings of discomfort or distress you’ve connected with caregiving.
- Remind yourself of the difficulties experienced by the person you care for — their pain and suffering.
- Allow these words of wisdom to drop into your awareness: Everyone is on their own life journey. I’m not the cause of this person’s suffering, nor is it completely within my power to make it go away, even though I wish I could. Moments like these are difficult to bear, yet I will try to help if I can.
- Notice and validate your own distress associated with being a caregiver.
- Put your attention on your in breath — breathe in compassion, understanding, warmth, and kindness for your own struggle as a caregiver. It’s hard.
- You also can imagine that you’re breathing in a golden, healing light that fills your body.
- Recall the image of the person you’re caring for and remind yourself of their struggle.
- As you breathe out, imagine that you’re breathing out compassion for the person you’re caring for and validating their pain. Breath out warmth, care, and concern. Imagine filling their body with a warm, golden light.
- Breathe in for yourself, breathe out for the person you’re caring for. “One for me, and one for you.”
- If you’re really struggling, change the ratio — breathe three in for yourself and one out for the other person.”
These suggestions may not resonate with everyone. But pick at least three from the list and give them a good try. Getting in touch with feelings about discomfort related to caregiving; self and others, and practicing breathing exercises are therapeutic. I know from experience that they do work.
Here is why breathing practices, meditation, and focused awareness work. When we are consistent in practicing a short, daily breathing technique, we learn to focus on our breath while observing thoughts that try to jump into the practice and take focus away from the breathing practice.
This is how we learn that we are not our thoughts, but we are the observer of our thoughts. Here is the bonus result, how that relates to stress:
When we are confronted with stress, we know that we are not the stress. We are the stress observer. Therefore; we can draw a circle around the stress and positioning ourselves outside the circle. This practice puts a distance between us and the stress. This allows us to see, feel, and respond, rather than melting into the stress.
Stress can be managed with self-care that includes stress management techniques. At any age, anyone can do this with consistent practice. Yet, we know there are days that we fall between the cracks; both when self-nursing and hospital nursing.
A day in the life of a nurse
There are days in a nurse’s life, and in our private life, when these suggestions may not be immediately doable because the sympathetic nervous system is in overdrive. When a nurse’s assignment is so unbelievable, unbelievably chaotic and overwhelming that only another nurse could understand the implications of what she endured, work engagement becomes harder.
The World Health Organization (WHO) informs us that there are 29 million nurses globally. Across the world, most nurses perform their duties above and beyond excellence, often with an empty stomach and a full bladder.
Their daily work is worthy of a Nobel prize nomination, unbeknownst to the 8+ billion people in the world who depend on their services. A day’s shift may look something like the following scenario.
In this mock hospital shift scenario, one nurse takes care of three patients. “Only three, big deal”, you may think, but think again.
Patient one is recovering from super high blood sugar (Hyperglycemia), receiving intravenous fluids, and is on an insulin drip, adjusted as per protocol. He needs frequent blood sugar monitoring and, at times, additional insulin injections, according to the physician’s orders.
Patient two is in isolation. He is on contact precautions for Clostridium Difficile (C.-diff) and needs assistance with frequent visits to the bedside commode.
Patient three is a stroke patient, on fall precautions. She is restless and repeatedly moves her unaffected arm and leg over the bedside rail.
One nurse assistant is on break, and the other nurse assistant is busy, turning patients. The nurse is then told that the stroke patient is up for transfer. Another patient is in the emergency room (ER), waiting for a bed. Adrenalin and silent despair run the show.
This is enough to put any nurse over the cliff. String a few of these days together, and burnout is lurking around the corner. Consecutive days of feeling overwhelmed, for whatever reason, must be interrupted to save nurses and older adults from burnout and generalized fatigue.
I remember one over-the-moon helpful practice that we adopted on my unit. The huddle prevented many a nurse’s nervous breakdown and burnout.
An overwhelmed nurse, like the one in the mock scenario, could call for a brief or a huddle. Call it an emergency team meeting with the nurses on the unit. The huddle was called to discuss and deal with immediate patient safety and workflow concerns for the nurse. Nurse to nurse, we took loads off each other’s backs and helped each other.
Create your own huddle. Asking for help is a sign of strength, not weakness. Neighbors, family, and friends can create a safety net of support for us as we grow older. Only a person practicing self-compassion will ask for help, rather than sinking from feeling overwhelmed.
At times, we must relieve ourselves from duties and responsibilities by reducing our own workload. This, I also learned from experience, fresh from a recent memory.
Life suddenly served this 75-year-old Norwegian an unexpected surprise
People in my age group may be old, but not me. Somehow, I escaped the aging thing. I saw myself as a strong, mature woman of my best age, but never old. That pseudo self-image fell apart less than two months ago, when I experienced a full-blown panic attack at a Wellness Center.
This scary experience was brought on by stress, while sitting in a waiting room with other old people, waiting to be called for scheduled diagnostic testing, including a treadmill stress test.
I had an epic; life changing experience in the waiting room at Cleveland Clinic. It was the first time that it dawned on me that I am in fact an old person. The next thought hit me fast and hard; old people get sick and die. That thought was followed by an instant panic attack. My resting heart rate and my resting blood pressure numbers shot through the roof.
Finding self-compassion in the aftermath of a traumatic stress test.
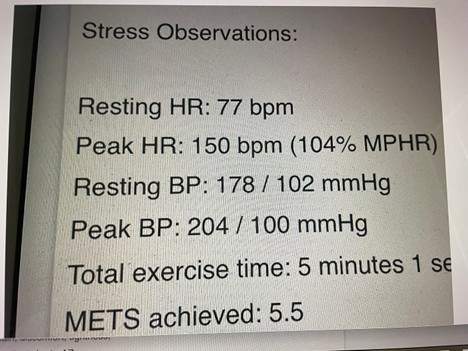
By the grace of the Universe, I did survive the stress test. At some point during the ordeal, I thought I would drop dead. Feeling short of breath, and as if my heart was exploding at a max heart rate (HR) of 150 beats per minute (bpm), I feared I was dying from an acute heart attack, like my Dad did at age 41. The following second, with a max blood pressure at 204/100 mmHg, I thought I would have a stroke, like my Mom did at age 64.
Elevated blood pressure (BP) and elevated heart rate (HR) are considered normal during a stress test. This is actually a good thing, evaluating the maximum tolerance of the heart during hard work. But because I was stressed out, my resting BP and my resting HR were way higher than normal and too high for me.
The [American Heart Association (AHA)](https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/all-about-heart-rate-pulse}[Opens new window.], tells us that a normal resting heart rate is between 60–100 bpm. Mine is normally in the 60s, dipping down to the 50s when at rest. Pre-stress test, my resting HR was 77. Although normal, it is too high for me.
The AHA also tells us that the ideal normal BP should be below 120/80 mmHg. Mine was waaaaay too high, stress-related and recorded at 172/102 mmHg.
When the testing was completed, the nurse managing the stress test guided me through breathing techniques in order to calm me down. Because I was still in a sympathetic overdrive, it was hard. But I stood with it, on and off. Eventually, I did move out of my stress-induced panic attack.
Driving home, still feeling anxious about my BP, I decided that my mindset and my daily routine needed a tune-up.
- First, I decided to cut myself some slack. Instead of stopping at the grocery store and preparing for a family dinner gathering planned for the same evening, I canceled it. That was not easy.
- Second, I came into full acceptance that a woman who has lived for 75 years is indeed old. And that is a good thing, a privilege not awarded to everyone. If I get sick, I will handle it, as I have handled everything else in my life; one thing and one day at a time.
- I also decided that I will never again have another stress test. Then I told myself, “ Dear Annelie, you got this. Relax your age-related standards and go with the flow. Do what you can, without performance anxiety.”
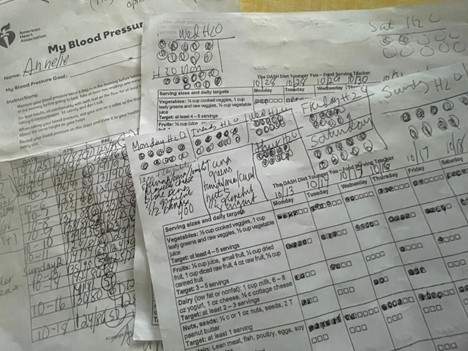
- I decided that doing what I can would include trying to achieve a therapeutic BP, by seriously complying with the Dietary Approach to Stop Hypertension (DASH) diet eating plan. I have been on this diet for more than 10 years. BUT only as it was convenient for me. I decided to comply with the servings; numbers and sizes, and document my daily intake, without lying to myself.
- I decided to honor myself; provide self-compassion and self-care as my 75-year-old self deserved. I decided to make a list of the things that deserve my priorities; self, family, entertainment, friends, pleasures, and health-oriented practices that will keep me rocking long enough to watch my grandchildren grow up.
Dear reader, nurse thyself; by providing enough self-compassion to elevate the quality, and hopefully, quantity of life.
Understand that you are one of a kind, and that you deserve the best of what life has to offer. If you are over 65, chill out. Don’t take life too seriously, but take yourself seriously. None of us is getting out of this life alive. Try to avoid what brings pain, like self-criticism and too high self-expectations. Learn to say NO to things that sink you, and YES to what empower you. Enjoy what brings pleasure; what matters to your well-being. Because only YOU are the expert on what your needs and wants are, only you can create a daily routine that supports and nurses your best self.
Bring awareness to what matters, and keep your body, your mind, and your spirit intact. Know that the thoughts you put in your mind shape your life. Remember; you are not your thoughts, you are the director of your thoughts. Make them useful. The flip side of that token; when stress comes your way, remember that you are not the stress. Respond to the stress, rather than react into panic or anxiety, like yours truly.
You cannot live without your body. Your body is build, cell by cell, from the food you ingest. Make it good. Remember; input shapes the output. Healthy foods produce good energy. Processed and low quality diet intake, results in poor output as it relates to health and energy. Junk in equals junk out.
Your spirit makes you who you are. It anchors you to the earth. Discover, develop, enjoy, and share your personal attributes, the ones that make you feel happy. Your unique abilities set you apart from the eight + billion people that we share the world with. No one can do exactly what you can do, the way you do it.
Take care of yourself and take care of the people you love. We could die at any time, regardless of doing everything right. Growing old is a privilege, it is not a birthright. Be of service to yourself and the people around you. Until your time comes, do your best to nurture your own being.
Knowing how to do something does not automatically mean that we are going to do that something. Don’t be too hard on yourself when you mess up; we all do.
Humans stumble and fall to unimaginable lows with sorrow and woe. Then, unexpected and sudden, we discover delight and bliss around the corner.
It’s just how life works sometimes, in our world.
Lucky for us, aging does not come alone. It brings hard earned lessons and wisdom along. Nothing in life is certain. But I believe this to be more true than false;
By positively nursing ourselves through the aging process, chances are that we will stay afloat longer and better with our physical, mental, and spiritual faculties intact.
Thank you ♥️
. . .
Annelie Holmene Pelaez believes that everyone has an attribute to share with others. Promoting cardiovascular health and helping adults over age 65 is her contribution. When we don’t let age define us, but rather empower us to grow, we discover health and happiness are byproducts of who we are.
Annelie is the author of the book, Say Yes to A Better Life, available at Amazon.
Sign up for our newsletter and a free PDF designed specifically for Boomer Girls.
Some of the links on this website are affiliate links, which means I may earn a small commission if you make a purchase through these links, at no extra cost to you. I only recommend products and services that I believe in and think will add value to my readers. Your support by using these links helps to keep the site running and allows me to continue offering helpful content.





